Best Study on Vegan Protein Intakes to Date
January 31st, 2016 by Jack Norris RDI just updated the Protein page at VeganHealth.org with a new section, Intakes and Plasma Amino Acid Levels in Vegans, based on a recent study from EPIC-Oxford.
The new research cannot substitute for a nitrogen balance or protein synthesis study on vegans, which I have been hoping to see, but for now it’s what we have.
The takeaway message is that vegans, and particularly vegan women, should continue to make sure they eat plenty of lysine-rich foods, and that if you do, you should be covering all your protein needs.
I have reproduced the new section below.
Intakes and Plasma Amino Acid Levels in Vegans
A 2015 report from EPIC-Oxford analyzed the dietary intakes and blood levels of amino acids in various diet groups in adult men (15). The study included 98 men for each diet group (vegan, lacto-ovo, pesco, and meat-eater). The authors say, “[T]his is the largest study to date of amino acids in the circulation or in the diet by habitual diet group, and on average participants had followed their diet for several years.”
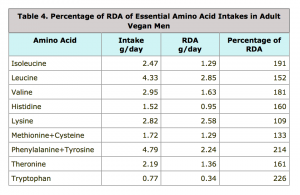
RDA
The study didn’t compare the intakes of the various diet groups to the US RDA for amino acids, but I have done so in Table 4 below.
Vegan men met the RDA for all essential amino acids.
This study bolstered the idea that lysine is the limiting amino acid in vegan diets, with vegan men surpassing the RDA by the lowest amount–9%. Methionine, the amino acid of second most concern, surpassed the RDA at the next lowest level of 33%.
The 95% confidence interval for lysine was 2.69-2.95 g/day; with the lower margin coming in at 104% of the RDA. The people on the lower end might have been the people who weighed less (and thus had a lower RDA than the average vegan).
The RDA for protein and amino acids is the same for women as it is for men (based on a percentage of their body weight). Male vegans in EPIC-Oxford were found to eat 10.7% more protein than female vegans (62 vs. 56 g per day; link). If you assume female vegans eat the same percentage of high-lysine foods as men, their average lysine intakes would be only 98.7% of the RDA.
Given that women have a lower percentage of lean body mass on average, it might seem curious that they have the same RDA for protein (and amino acids). In determining the RDAs, the Institute of Medicine says (Ref 2, p. 644):
Although the data indicate that women have a lower nitrogen requirement than men per kilogram of body weight, this was only statistically significant when all studies were included, but not when the analysis was restricted to the primary data sets. This difference may be due to differences in body composition between men and women, with women and men having on average 28 and 15 percent fat mass, respectively. When controlled for lean body mass, no gender differences in the protein requirements were found. However, in view of the uncertain significance of the difference between the genders, the same protein EAR [i.e., Estimated Average Requirement, a foundation for the RDA] on a body weight basis for both men and women is chosen.
Another consideration is that the vegans in the UK may eat lower amounts of protein than those in the U.S. Adventist Health Study-2 found an average protein intake of 71 g/day for men and women combined, considerably more than in EPIC-OXford (link). It seems safe to assume that Seventh Day Adventist woman are likely getting plenty of lysine and other amino acids.
Finally, according to the authors, “[T]he validation of the [food frequency questionnaire] showed that protein intake was particularly difficult to estimate.”
Blood Levels
In comparing blood levels of amino acids between diet groups, vegans had lower levels of lysine, methionine, tryptophan, and tyrosine, and higher levels of alanine and glycine.
Interestingly, arginine, a dietary concern for vegans with herpes virus, was actually lower in the blood of vegans, but not significantly. It was also lower in the diet (3.92 g/day for vegans vs. 4.13 g/day for meat-eaters; lacto-ovo vegetarians had the lowest intake at 3.36 g/day).
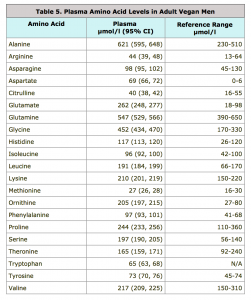
The authors didn’t seem alarmed by any of the differences found between diet groups. I decided to take things a bit further and compare the plasma levels found in this study to the reference ranges given by the U.S. National Library of Medicine in Table 5 below.
In comparing the vegan’s blood levels to the reference range:
- Alanine, glutamate, glycine, leucine, ornithine (a non-protein amino acid), phenylalanine, and serine are higher.
- Aspartate is also higher, but the reference range is curiously low.
- There is no reference range for tryptophan, with no explanation as to why.
- There is a reference range for cystine (which is two cysteine molecules combined), but EPIC-Oxford didn’t list plasma levels for cystine or cysteine.
It is not clear what any of this means and the U.S. Library of Science notes that these numbers are dependent on the specific laboratory methods used.
Conclusion
The above research is not a great substitute for a nitrogen or protein synthesis study on vegans, but for now it’s what we have. The takeaway message is that vegans, and particularly vegan women, should continue to make sure they eat plenty of lysine-rich foods. There is no reason to think that the vegans in this study were aware of lysine or trying to increase their lysine intakes, so any vegan who does so should be well covered.
Support JackNorrisRd.com
If you like my posts, please like my posts! Or share them!
I am very grateful for donations of any amount (click here).
Purchase anything through these links and JackNorrisRD.com gets a percentage:
– Pangea – The Vegan Store
– Amazon.com
– Vegan for Life by Jack Norris & Ginny Messina
Thank you!
References
2. Dietary Reference Intakes: Macronutrients. National Academy of Sciences. Institute of Medicine. Food and Nutrition Board. DRI table for carbohydrate, fiber, fat, fatty acids and protein. | PDF
15. Schmidt JA, Rinaldi S, Scalbert A, Ferrari P, Achaintre D, Gunter MJ, Appleby PN, Key TJ, Travis RC. Plasma concentrations and intakes of amino acids in male meat-eaters, fish-eaters, vegetarians and vegans: a cross-sectional analysis in the EPIC-Oxford cohort. Eur J Clin Nutr. 2015 Sep 23. | link
16. Plasma amino acids. Medline Plus. U.S. National Library of Medicine. Accessed January 30, 2016. | link